Post diagnosis of 22q11.2 Deletion Syndrome, Harrison continued to catch some virulent chest infections that took him weeks to recover from. This meant that planned social activities were regularly cancelled sometimes at very short notice. When he wasn't in hospital, we usually had at least three therapy or doctors' appointments per week. It was a full-time job looking after Harrison and there was no way that I could contemplate working; not even part time!
Getting out of the house to the appointments was a mammoth mission, so I'll save that for another post!
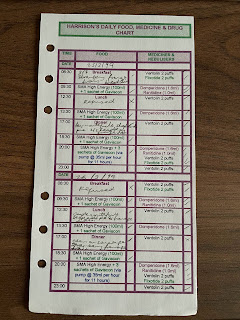
Harrison's feeding, medicine and appointment regime was relentless. I've already hinted at this in a previous post but here's a glimpse into our life at that time. I had to keep everything in a Filofax to keep me on track. Nowadays, smartphones, apps and the like make everything so much more manageable. Below is a sample of his basic food and medicine chart where I tried to capture his meals and usual medications. Although he was 14 months old according to this page, I found this one still in my Filofax the other day! This was the chart that I used when we were travelling to, at, or on our way home from appointments. It was all transferred to a much more comprehensive sheet where the inevitable additional antibiotics and other ad hoc prescribed medications were detailed, and volumes out were estimated. Keeping these records helped me to give as much information as possible to the doctors and dieticians looking after him. There was no way I could remember everything without writing it all down!
Seeing it here doesn't make it look very time consuming. However, what I haven't recorded was the length of time it took to coax Harrison into eating two thirds of a fromage frais! Breakfast would regularly run into the time for his first 100mls of SMA High Energy milk. This wasn't so much of an issue because that was all given via his feeding tube however, it had to be for a specific amount of time. If we were lucky, we could usually squeeze the milk feed into an hour. It needed to be very slow otherwise the whole feed would come back! In addition to creating extra work for me cleaning everything up, that would be another few hundred calories (and probably some medications) that wouldn't have been absorbed. Switching to the high energy formula was a win on two fronts:
- Not quite as stressful trying to get volume into (and remain in!) Harrison because containing 1 1/2 calories per millilitre he needed less of it;
- It was ready made up and was stored at room temperature, so it became super easy to prepare Harrison's feeds with his demanding schedule. No measuring of powder or cooled boiled water required.
Following each formula feed though, Harrison then had to be restrained and entertained in his highchair for another hour to give his body a chance to hang onto what went in! Can you imagine the disappointment and frustration when you think that you've cracked it but inadvertently allow Harrison freedom a few minutes earlier than you know you should (because his demeanour is showing that he's okay), only to be proved wrong and the carpet, highchair and Harrison's clothes all get another soaking in undigested formula?
There were surely easier ways for Harrison to tell us that he didn't like our choice of carpet and would prefer a hard floor instead! So by now, we're at 10:30am and depending on how optimistic I was feeling, I may or may not have dressed Harrison prior to that feed!
The feeding and medication routine was priority 24 /7 and the rest of our lives had to fit around it. The mandatory weigh-ins three times a week plus the daily weight checks when in hospital, meant that we soon needed additional pages added to the weight section of Harrison's red book.
Sleep for us continued to be a luxury because we had to go to bed late and get up during the night to tube feed Harrison. Those first few weeks of having a new baby and feeding through the night dragged on for months because he was unable to tolerate a 'normal' volume of feed in one sitting. We'd experienced countless stays on the children's ward and every night I'd ask the night staff to wake me at specific times so that I could tube feed Harrison. One night, a very perceptive nurse asked why I didn't use a feeding pump. I had no idea what she was talking about! She left the room and returned with my life saver! An electronic pump that the staff could set up and programme to deliver Harrison's overnight feeds without waking me up!! I felt like I'd won the lottery! From then on, night times in hospital were far more pleasant and I started to feel human again. Obviously, that all went out the window if Harrison was unwell or deteriorated during the night.
Even in the short period of the first few months of Harrison's life, caring for a sick baby was extremely exhausting and I was completely burnt out. We didn't qualify for help from social services because we appeared to be coping. That was so far from the truth. I was existing and floundering aimlessly in a foggy cloud from one day to the next. Things first came to a head during one of Harrison's almost fortnightly inpatients stays in our local hospital when he was about six months old. For a few weeks we'd been trying a more frequent feeding regime which as I mentioned previously, took around an hour at a time. This was relentless day and night and came to a head when I passed out from exhaustion on the ward. The impression everybody had that I was coping was clearly wrong. The nursing staff immediately took charge and sent me home for bed rest. I hadn't spent a single night apart from Harrison since he was born. I initially resisted but knew I needed a break. The staff assured me that Harrison would be assigned a personal nurse who would step into my role until I was fit to resume, and then they banned me from the ward for three days to enforce me to rest. I only managed one! Even just 24 hours rest had a massive impact on my ability to cope again. There was no protocol for this support, the nurses were just responsive to my needs.
A few months later a similar situation occurred when the nursing community team came to do their bi-weekly check on Harrison at home. I happened to be in the kitchen preparing his feed but I could barely stand up as I was so tired. Again, they sent me upstairs to rest and although they were only supposed to be with me for about 20 minutes, they stayed for three hours until my husband got home from work and could take over from them.
After that, the team took it upon themselves to organise a rota of two hourly respite once a week for me, in their own time. Although we didn’t qualify as a family, it was obvious that I needed help. Our local nursing team have been more than just carers for Harrison; they cared for our whole family.



No comments:
Post a Comment